Beth Sandy, MSN, CRNP
Sharon is a 55-year-old woman with limited-stage small cell lung cancer (SCLC). She is in the emergency room (ER) at her local hospital due to dehydration from poor oral intake associated with the chemotherapy and radiation treatments. The doctor assigned to her stands in the doorway of her room with 4 medical residents and students and begins to present her clinical case to the team. He starts out by saying, “Here in room 10, we have the small cell with dehydration ….”
This type of language happens all too frequently in medicine. While it is not appropriate in any sector of medicine, it is especially degrading to patients who have cancer. Sharon is my patient. She told me about this encounter in a follow-up office visit, through tears, expressing how minimized and marginalized she felt at that moment. Being referred to as a “small cell” completely dehumanized her. She felt a lack of trust, a lack of caring, and, also at that moment, a lack of confidence in her medical team in that ER.
How we speak to our patients, and their family members, matters. A patient’s cancer does not define who they are. Their cancer is its own disease process that will act in a unique way for each patient. It matters not only when we address patients directly or within earshot, as was the case in this clinical scenario, but it also matters when we discuss patients and cancer among colleagues, in presentations, and in everyday life. Appropriate language is not just a statement; it is the way the world should view patients and their illness, as separate entities, yet intertwined.
Mental health counselors have been publishing about this “labeling” effect on their patients in recent years. There is little research to evaluate how the use of labels to identify a patient can cause negative effects; however, in mental health circles, patients with schizophrenia have often been referred to in a negative light as “schizophrenics,” “schizo,” or “the mentally ill”. One study demonstrated that mental health counselors had kinder and less authoritative reactions to statements that used the phrase “person with schizophrenia” as opposed to statements that labeled the patient as “schizophrenic.”1
What can we do as oncology providers? We need to be respectful of patients, their families, and other healthcare professionals. The Table (below) lists examples of changes we can make in everyday language when referring to patients.
Table. Wrong Language Versus Correct Language2
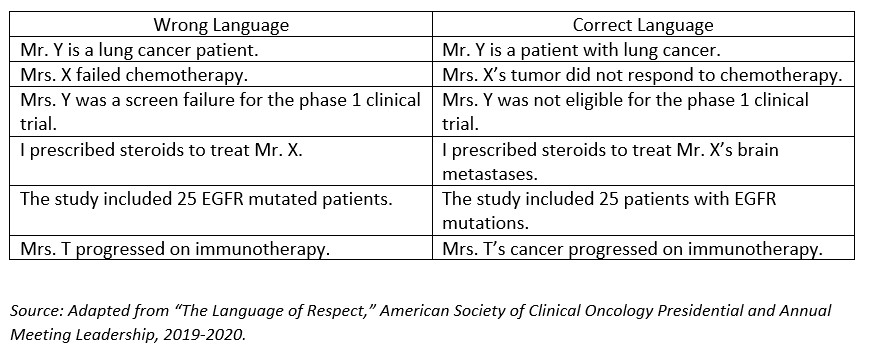
We need to address patients by name and never label them or refer to them by their diagnosis. It is very important to say, “Your lung cancer worsened on immunotherapy” as opposed to the more accusatory statement, “You progressed on immunotherapy.” We must be sure to speak with respect and avoid language that blames the patient or dehumanizes the individual with cancer. Clinicians and oncology providers must practice our due diligence by using appropriate language when discussing our patients so as to treat our patients with respect and serve as role models for our emerging generation of nurses and doctors.
Beth Sandy, MSN, CRNP is a thoracic oncology nurse practitioner at Abramson Cancer Center, University of Pennsylvania, Philadelphia. She is the editor-in-chief of The Oncology Connection.
References
- Granello, D.H. and Gorby, S.R. (2021), It’s time for counselors to modify our language: It matters when we call our clients schizophrenics versus people with schizophrenia. Journal of Counseling & Development, 99(4), 452-461.
- The Language of Respect,” American Society of Clinical Oncology Presidential and Annual Meeting Leadership, 2019-2020. https://s3.amazonaws.com/files.oncologymeetings.org/prod/s3fs-public/2019-12/The_Language_Of_Respect-Final-12-09-2019.pdf
For more information
Duma N., Durani U., Woods, C. B., Kankeu Fonkoua, L. A., Cook, J. M. Wee C. … Knoll, M. A. (2019). Evaluating unconscious bias: Speaker introductions at an international oncology conference. Journal Clinical Oncology, 37(36), 3538-3545.
International Association for the Study of Lung Cancer. Language Guide. https://www.iaslc.org/IASLCLanguageGuide

Thoracic Oncology Nurse Practitioner
Abramson Cancer Center, University of Pennsylvania
Philadelphia, PA