Mohamud Ali, PharmD
Cardio-oncology is a growing field focusing on the overlap between cardiovascular health and cancer care. Medications used for cancer treatment can have various effects on the cardiovascular system. Some drugs, like doxorubicin, cyclophosphamide, and trastuzumab, directly affect the heart’s functioning, leading to issues such as left ventricular (LV) dysfunction and arrythmias. Others influence heart health indirectly, involving aspects such as fluid retention, blood pressure, and heart rate, seen with drugs such as imatinib and bevacizumab. These indirect effects can result in conditions such as hypertension, heart failure, and increased risk of thromboembolism.
To foster the growth of the cardio-oncologic specialty, guidelines and educational opportunities have become more available for those involved and interested in this area. Building on previous oncologic guidelines from organizations such as the American Society of Clinical Oncology (ASCO) and the European Society for Medical Oncology (ESMO), the new European Society of Cardiology (ESC) guidelines aim to address existing gaps and provide a more comprehensive approach. In this interview, we discuss and apply the latest ESC guidelines in this context with Tochukwu Okwuosa, DO, lead cardiologist at Rush University Medical Center, Chicago, IL, where she also serves as a Professor of Medicine and Cardiology. Her specialization is in cardio-oncology, and her research emphasizes preventive cardio-oncology. Additionally, she founded the Chicago Citywide Cardio-Oncology Consortium, where practitioners from around Chicago convene quarterly to discuss cases, management techniques, and research collaborations.
Cardiotoxicity Differentiation and Management
Thank you for your time today, Dr Okwuosa. The predominant cancer therapy-related cardiotoxicities seem to involve LV function stemming from anthracyclines and QT prolongation from drugs like tyrosine kinase inhibitors. Which toxicities are most prevalent in your practice, and which agents tend to be the main culprits?
Dr Okwuosa: If we’re talking about cardiac-specific toxicity, I would say LV dysfunction/cardiomyopathy and arrhythmias. If we’re talking about broader cardiovascular toxicity, hypertension is a significant concern. A lot of oncologic drugs can induce hypertension, and a lot of our Rush oncologists are realizing this now based on my presentations. While anthracyclines are commonly associated with cardiotoxicity, a broader range of drugs and treatments need to be considered in cardio-oncology.
When cancer patients are treated with anthracycline-based medications, they are at a much greater risk of developing heart failure, typically 3 to 5 times more likely, compared to other heart-related issues. If they have uncontrolled hypertension, oncologists take note. They will typically consult with the patient’s primary care doctor first. But if the hypertension is not controlled adequately, they might refer the patient to a specialist.
Specific agents like vascular endothelial growth factor (VEGF) inhibitors increase the risk of hypertension. I’ve seen blood pressures reaching 250 mmHg with some of these drugs, which is concerning. Such elevated pressures can lead patients to the emergency room with complications. We can’t solely attribute these risks to LV function. Hypertension and QT prolongation also play a role. Another issue is arrhythmias, especially atrial fibrillation (Afib). Many don’t consider this, but it’s a significant concern with some drug classes. Afib is more common than most realize, and recent cardiological studies are shedding light on its risks, especially in cancer patients and survivors.
I’ve heard from clinicians that differentiating cardiotoxicity from oncologic treatments and existing cardiovascular diseases (CVD) is a common challenge. In your experience, how do you manage this?
Dr Okwuosa: It is a continuum. If a patient has existing CVD, they are more susceptible to complications during cancer treatment. Hence, early referral is crucial. For example, I’ve seen some patients start oncological treatment and suddenly develop heart failure. And then you’re looking for that baseline echocardiogram to determine if the ejection fraction (EF) was normal or abnormal before cancer treatment, and you don’t find a baseline echocardiogram.
Similarly, a baseline electrocardiogram (EKG) is essential for those who develop arrhythmias during treatment. Acquiring these baseline data can significantly help in distinguishing between the two conditions.
To follow up on that, are you seeing more patients for preemptive assessments before they begin therapy rather than waiting for an issue to arise during treatment?
Dr Okwuosa: Initially, most referrals were reactive—patients already showing signs of cardiotoxicity. But as awareness grows, we’re shifting towards preventive evaluations. It’s more efficient for us to assess and clear patients at the outset rather than dealing with complications down the line. If we identify no significant concerns or risk factors, we can assure the oncology team and only step in if an issue arises later. This proactive strategy reduces treatment disruptions and offers a better overall patient experience.
Patient Case Application
Jane, a 52-year-old patient with hormone receptor (HR)-positive/HER2-negative stage IIA breast cancer (pT2N0M0), underwent a left total mastectomy. Adjuvant treatment plan: AC (doxorubicin 60mg/m2 + cyclophosphamide 600mg/m2) x 4 cycles, paclitaxel 175mg/m2 x 4 cycles, then tamoxifen 20 mg PO daily for 5 to 10 years.
- Chief complaint: She presents to the clinic today for evaluation before next cycle of chemotherapy. She worries about her new symptoms (shortness of breath, palpitations, chest discomfort, ankle swelling) and how they might relate to her ongoing breast cancer treatment.
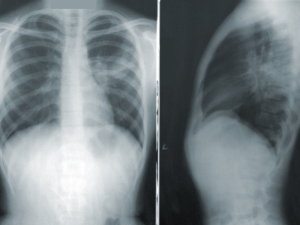
- Echocardiogram – Left ventricular ejection fraction (LVEF) 50% on today’s visit (baseline was 60%). Her blood pressure is normal.
- Blood tests: Elevated B-type natriuretic peptide (BNP) levels, normal electrolytes, liver and renal function.
- Family history: Jane’s mother suffered from heart failure in her late 60s, and her paternal grandfather had a myocardial infarction in his 50s.
- Past medical history: Hypertension, managed with amlodipine 5 mg daily.
- Current medication regimen: Amlodipine 5 mg daily, doxorubicin 60 mg/m2, cyclophosphamide 600 mg/m2, paclitaxel 175 mg/m2, and occasional use of dexamethasone during chemotherapy cycles.
We have a case study here; let’s discuss our patient, Jane. She’s experiencing discomfort in her left chest region, shortness of breath, and occasional palpitations posttreatment. She also noticed swelling in her ankles by the end of the day. Her laboratory studies show a reduced LVEF to 50%, elevated BNP levels, and normal liver function. She is concerned about the impact of her new symptoms on her ongoing breast cancer treatment. Looking at her treatment regimen, would you recommend any adjustments or further tests?
Dr Okwuosa: Given the patient’s symptoms and findings, my approach would prioritize guideline-directed medical therapy. It’s worth noting that shortness of breath and fatigue could be indicative of cardiomyopathy, heart failure, or even pulmonary embolism, but it could also be a result of something else, like constipation or anemia, which is common during cancer treatment. So, I always assess the patient as a whole to help determine the etiology of their presenting symptoms.
The other big thing is hypovolemia, which is a concern for cancer patients due to factors like nausea, vomiting, loss of appetite, and increased cell turnover. While we encourage hydration, not all patients can maintain adequate intake. If her decreased LVEF is related to her cancer therapy, I would consider adjusting her medications by switching her to guideline-directed medical therapy, like a beta-blocker or an angiotensin-converting enzyme (ACE) inhibitor for blood pressure management. And then of course, I would reimage over the next couple of months just to see if there’s been an improvement.
We should also check for global longitudinal strain, which offers insights into LV function. Even if someone has a normal ejection fraction post-treatment, a significant drop in strain could signify potential cardiotoxicity or future risk. We must also decipher the cause of the elevated BNP, whether it’s due to kidney function, cardiotoxicity, or arrhythmias. In addition to strain and BNP, I often check troponins to assess risk during treatment; then focusing on BNP and strain post-treatment. There’s a lot of thought process that goes into thinking through these patients and how to best manage them.
You mentioned the importance of blood pressure. This patient has normal blood pressure. How would you address her hypertension regimen if her pressure was elevated around stage 2 or even 200/140?
Dr Okwuosa: With elevated blood pressure, particularly during anthracycline treatment, my priority would be to ensure the patient is on guideline-directed medical therapy. While ACE inhibitors and beta-blockers are beneficial, they might not always adequately reduce the blood pressures. As per general cardiology guidelines, the next logical step would be diuretics, but I’m hesitant to prescribe them in these situations. Many patients undergoing cancer treatment face hypovolemia and adding a diuretic could further lower their blood pressure, exacerbating fatigue. Also, many of these patients experience electrolyte imbalances like hypokalemia and hypomagnesemia due to cancer treatments. Using medications like hydrochlorothiazide can worsen these imbalances. That’s the challenge with cardio-oncology; general cardiology guidelines might not always be ideal. In such cases as this one, I would lean towards calcium channel blockers, specifically the dihydropyridine class, as they effectively manage blood pressure without the risk of drug interactions associated with cancer therapies.
Regarding drug interactions, are there any ones you watch out for?
Dr Okwuosa: Absolutely. Due to their potential interactions with cancer therapies, I would avoid non-dihydropyridine calcium channel blockers like diltiazem. Instead, I’d opt for dihydropyridines like amlodipine, but with the caveat that patients might experience lower extremity edema as a side effect.
Patient Journey and Transitions of Care
Regarding the patient journey, the guidelines reference the term “care tracks” or pathways tailored for cancer patients. These pathways in cardio-oncology services aim to minimize delays in examinations and treatment decisions. I came across an interesting study suggesting that the risk of long-term cardiotoxicity multiplies for every subsequent 2-month delay. From your perspective, when should a patient ideally be referred to cardio-oncology?
Dr Okwuosa: At Rush, we use a reference document called the Ramp Rush Algorithms for managing cardiac cancer patients. This document outlines various algorithms based on the type of cancer treatment, helping to determine the right time to consider referring patients to cardio-oncology. Generally, there are 3 key categories: pre-treatment, during, and post-treatment.
Before treatment, patients with known cardiovascular risk factors, especially those scheduled for potentially cardiotoxic therapies, should be considered for referral. For instance, if a baseline EKG or echocardiogram reveals an unexplained abnormality and a cardiotoxic treatment is planned, a referral makes sense.
The second category is patients undergoing treatment. They should be referred if they develop any cardiovascular issues during this phase, even if the link to the treatment is unclear. An example would be a patient undergoing a specific therapy who starts experiencing chest pains or has a reduced ejection fraction noted in an emergency room evaluation.
The final category encompasses cancer survivors who have undergone potentially cardiotoxic treatments, such as high-dose radiation or certain medications, and those living with metastatic disease requiring ongoing cancer treatments. Due to advancements in cancer treatment, these patients often live much longer and are thus exposed to potential cardiotoxicities over extended periods. Patients with metastatic diseases now live longer, sometimes 20 to 25 years, because of advancements in treatments. As these treatments change based on their response, it’s important to consistently evaluate the potential cardiotoxicities of these treatments and their long-term impact.

Mohamud Ali, PharmD, is a freelance medical writer.
For more information:
Alexandre, J., Cautela, J., Ederhy, S., Damaj, G. L., Salem, J. E., Barlesi, F., Farnault, L., Charbonnier, A., Mirabel, M., Champiat, S., Cohen-Solal, A., Cohen, A., Dolladille, C., & Thuny, F. (2020). Cardiovascular Toxicity Related to Cancer Treatment: A Pragmatic Approach to the American and European Cardio-Oncology Guidelines. Journal of the American Heart Association, 9(18), e018403.