Integrating geriatric principles into routine oncology practice can improve care for older patients with cancer, according to Leah Witt Gaspard, MD, an assistant professor of geriatrics and pulmonary medicine, at UCSF, San Francisco, CA. Witt Gaspard, a pulmonologist and geriatrician, is on a mission to infiltrate every subspecialty with the principles of care for older adults that might not have been taught during training for the profession.
“Providers who have some expertise in geriatric principles become ‘geriatricized,’ and they will provide better care for older adults,” said Witt Gaspard who spoke at the Advanced Practice Provider Oncology Summit (APPOS) in San Francisco held in August. “A core message that I share is that geriatricians are an important part of the solution, but they are not the solution because our geriatric workforce is just not big enough to take care of every adult,” she told The Oncology Connection.
Integrating geriatric principles into oncology is especially important because cancer is a disease of aging. The median age at cancer diagnosis is 67, and the median age at cancer death is 73. As the Baby Boomer generation (adults born 1946 to 1964) ages, the population that is 65 years of age and older is growing rapidly. “Our population is aging, and there is an urgent need for health care systems and specialists to meet their needs for health care,” Witt Gaspard said.
Principles of Geriatrics
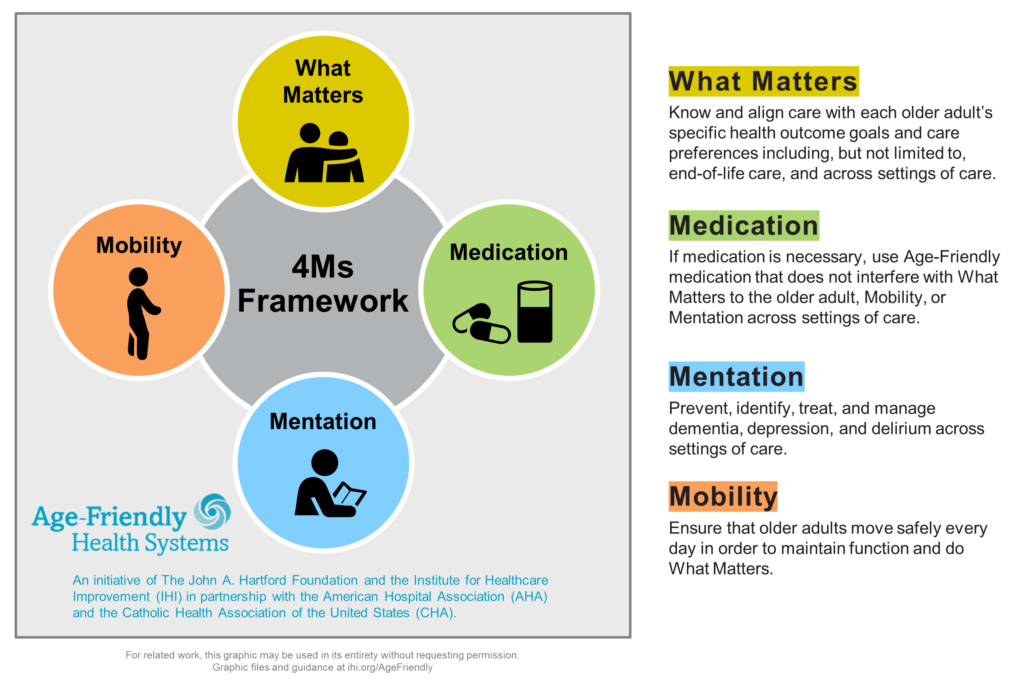
Geriatrics focuses on function and how disease affects social, emotional, and physical functioning, as well as how the patient’s environment can support function. Function affects quality of life and is a predictor of institutionalization and hospital mortality, Witt Gaspard explained. She uses the 4Ms—Medication, Mobility, What Matters, and Mentation—as a framework for teaching geriatrics to other providers (see Figure).
“You can think about each element and how it may apply to whatever disease you are managing,” she said, adding that she includes a fifth M. “The fifth M, multimorbidity, means all the other medical problems that people are dealing with,” she said. “Treating somebody’s cancer is not in a vacuum by itself without their other medical problems, like a history of stroke or diabetes.”
For the past three years Witt Gaspard has used the 4M framework in her geriatric consults for patients older than age 60 who were receiving an allogeneic stem cell transplant or patients older than 65 who were receiving an autologous stem cell transplant or chimeric antigen receptor (CAR) T cell therapy.
Clinical Trials
Since older adults are underrepresented in oncology clinical trials, Witt Gaspard advises providers to consider whether a clinical trial result applies to their older patients when selecting a treatment. “It is helpful to look at the methods and the inclusion and exclusion criteria,” she said.
She contrasted the characteristics of older patients that participate in clinical trials with those seen in the clinic. In oncology clinical trials, older patients are typically the fittest of the fit, have minimal or no comorbidities, their creatine clearance (CrCl) is higher than 60, no geriatric syndromes are present, and they have strong caregiver support. However, in the clinic, older patients are often vulnerable and frail, have multiple comorbidities, their CrCl is almost always less than 60, they have experienced multiple falls, and their caregiver support is variable.
The challenge then is how to individualize cancer care for fitness and adjust for vulnerable or frail patients. To determine a patient’s risk from traditional chemotherapy, Witt Gaspard recommends the Cancer and Aging Research Group (CARG) chemotherapy toxicity calculator, a validated pre-treatment assessment, to predict grade 3 or higher adverse events from chemotherapy in older adults.
Staging the Aging
Witt Gaspard recommends comprehensive geriatric assessments, including assessing for comorbidities, physical function, and cognitive/psychosocial evaluation, for older patients at risk for treatment toxicities. These assessments can be conducted by a physician, advanced care provider, or nurse trained in geriatric assessments.
Chronological age does not equal physiologic age; therefore, in addition to staging the patient’s cancer, Witt Gaspard stages the patient’s physiologic age and function. “That cancer’s stage is not the only thing that affects what your treatment plan is and what morbidity and mortality will be,” she said. Other factors include frailty, cognition, comorbidity, geriatric syndromes, caregiver support, social support, nutrition, goals of care, life expectancy, and functional status.
“Somebody’s functional status really impacts what their experience will be with the cancer, their morbidity and mortality, risk of toxicity from the treatments, and ultimately which treatment might be chosen,” she said.
People Living With Cancer
People living with cancer have several geriatrics care needs that can inform diagnosis and treatment. Frailty, functional impairment, medication problems (ie, financial, adherence and side effects), cognitive impairment/mental health issues and advance care planning are key issues, Witt Gaspard said.
In her geriatric consult practice, Witt Gaspard starts with a basic review of symptoms focused on geriatric systems or symptoms and then asks about medications, including prescriptions, over-the-counter medications, and supplements. She conducts a thorough cognitive assessment, which includes the caregiver for collateral history. A Mini Cog Mental Status Examination, which takes 3 minutes, is included in every visit. In addition, she asks patients about their mood and will recommend additional evaluation by their primary care provider or oncology team if there are concerns for mental health issues.
Many of Witt Gaspard’s exams are conducted virtually. For in-person visits, she will do a Short Physical Performance Battery, which includes physical maneuvers to evaluate a person’s functional status, such as a timed walk for 3 or 4 meters, timing a person’s ability to do 5 chair stands, as well as their ability to balance with their feet next to each other, one slightly in front of the other, and then tandem-like walking on a tightrope.
“These are ways that we can assess somebody physically, cognitively, and use the Ms to identify targeted interventions so they can get through the intended treatment as successfully as possible,” Witt Gaspard said.
Optimizing Treatment
One area of growth in geriatrics is helping older patients who are super-fit optimize even further. “I point them to the resources I know, but I think that we could do even better for people who want to age even more optimally so we’re not just targeting our interventions for people who are more at risk,” she said.
Witt Gaspard believes that developing an expertise in recognizing and evaluating cognitive impairment is important for every provider. “I think even mild cognitive impairment can be missed by people who have known a patient for so long and by caregivers and even their physicians,” she said. “If you identify cognitive impairment, then you know that person is at risk for increased delirium in a hospital and might be more sensitive to some medications.”
Noting that her clinic is called the Treatment Optimization Program and not the Geriatric Consult Clinic, Witt Gaspard said many patients resist the geriatric label. “There definitely is a stigma about the term ‘geriatric,’ but the intention is that we want to take good care of people who are older, and the definition of who is older is always changing,” she said.
For more information
Hurria, A., Togawa, K., Mohile, S. G., Owusu, C., Klepin, H. D., Gross, C. P., Lichtman, S. M., Gajra, A., Bhatia, S., Katheria, V., Klapper, S., Hansen, K., Ramani, R., Lachs, M., Wong, F. L., & Tew, W. P. (2011). Predicting chemotherapy toxicity in older adults with cancer: a prospective multicenter study. Journal of clinical oncology : official journal of the American Society of Clinical Oncology, 29(25), 3457–3465. https://doi.org/10.1200/JCO.2011.34.7625
Institute for Healthcare Improvement. Age-Friendly Health Systems Resources and News. https://www.ihi.org/age-friendly-health-systems-resources-and-news

Leah Witt Gaspard, MD – Assistant professor of geriatrics and pulmonary medicine, at UCSF, San Francisco, CA.







