Part 1 of a two-part series
Fertility Preservation Provides Options for Patients With Cancer
Fertility preservation is a meaningful and important part of survivorship for patients who are being treated for cancer, according Julie A. Messina, PA-C, a physician assistant at Rocky Mountain Cancer Centers in Colorado. Pre- and postpubertal males and females who want to preserve their fertility at the time of cancer diagnosis have several options.

Messina is a consultant for Enriching Communication Skills for Health Professionals in Oncofertility (ECHO), a National Cancer Institute-funded training program, and participates in the Oncofertility Consortium, an international, interdisciplinary initiative designed to address the complex health care and quality of life issues of young patients with cancer.
She became involved in fertility preservation as part of survivorship care 19 years ago while she was a PA working with Leonard S. Sender, MD, a leader in the field of fertility preservation for young adults at the University of California-Irvine and at Children’s Hospital of Orange County (CHOC). For patients undergoing cancer treatment at that time, fertility preservation was largely limited to sperm cryopreservation, and oocyte cryopreservation was considered experimental.
“I was seeing how difficult it was for them to deal with the consequences of impaired fertility or no fertility after undergoing cancer treatment. A lot of cancer survivors dealt with issues such as guilt,” Messina said in an interview with The Oncology Connection. “They felt like they should be grateful that they are alive, but they wanted more; they also wanted to be fertile and to have a family of their own.”
Messina went on to become the fertility champion at CHOC from 2010 to 2017, the co-principal investigator in the ovarian tissue cryopreservation protocol for fertility preservation for girls, and the principal investigator in the testicular tissue harvesting protocol for fertility preservation for boys.
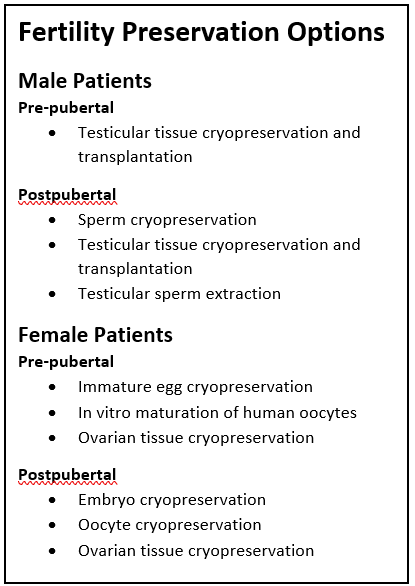
In addition to established options for postpubertal males and females, there are now experimental options for prepubertal patients as well. “Previously we really only could do fertility preservation in patients who had gone through puberty because prepubertal children didn’t have mature eggs, and they weren’t making sperm,” Messina said.
Fertility Preservation Options for Female Patients
Postpubertal females can freeze embryos, oocytes, and ovarian tissue cryopreservation (OTC). In OTC, ovarian tissue or the entire ovary is surgically removed and frozen. This tissue can be reimplanted or the eggs used for in vitro fertilization. In prepubertal females, OTC is considered experimental since the follicles are immature. Research on how to mature the follicles ex vivo is ongoing.
Oocyte harvesting and cryopreservation are typically reserved for patients whose cancer treatment can wait for 2 to 3 weeks while the patient is given follicle-stimulating medications, and then the oocytes are collected and frozen. Even in patients who are married, Messina said, reproductive endocrinologists recommend freezing embryos as well as oocytes to provide the patient with options. “If something happened to your partner or he decided not to let you use [the embryos] you also have eggs that you can use,” she explained.
Fertility Preservation Options for Male Patients
“For postpubertal males, the standard of care is sperm cryopreservation. After the sperm is collected by the patient, it is taken to the endocrinology reproductive center to be assessed and, if viable, frozen,” Messina explained. “Testicular sperm extraction (TESE) is an option for males who have gone through puberty but are unable to ejaculate sperm but may have live motile sperm in their testicle.” In TESE, which takes place in an operating room, a urologist extracts sperm from the epididymis. Also present is an embryologist who evaluates the sperm microscopically. If the sperm is alive and motile, it can be frozen as if the patient collected it themselves.
Prepubertal males who are not making sperm but have the spermatogonial stem cell intact can be offered an experimental procedure called testicular tissue cryopreservation. A wedge biopsy of the testes is obtained, and the tissue is sent to a research institution that freezes part of it for the patient and uses the rest for research in how to best freeze, thaw, and preserve the tissue as well as produce sperm from the spermatogonial stem cell in the laboratory.
“Unlike females who have all the eggs they are ever going to have, males can make more sperm as along as that stem cell isn’t damaged from their chemotherapy or radiation therapy, or from surgery, for example, if a patient has testicular cancer and it had to be removed. As of today, we haven’t successfully grown a sperm from the stem cell—that’s part of the research,” Messina said. “This is the future. I’m confident we’re going to have that ability at some point.”
Part 2: How to Talk About Fertility Options With Patients and Their Parents will be published in The Oncology Connection’s summer issue.
For more information
Enriching Communication Skills for Health Professionals in Oncofertility (ECHO). https://echotorch.org/
National Comprehensive Cancer Network. (2023). National Comprehensive Cancer Network Guidelines – Adolescent and Young Adult (AYA) Oncology. https://www.nccn.org/professionals/physician_gls/pdf/aya.pdf
Oktay, K., Harvey, B. E., Partridge, A. H., Quinn, G. P., Reinecke, J., Taylor, H. S., Wallace, W. H., Wang, E. T., & Loren, A. W. (2018). Fertility preservation in patients with cancer: ASCO Clinical Practice Guideline Update. Journal of Clinical Oncology: An American Society of Clinical Oncology Journal, 36(19), 1994–2001.
The Oncofertility Consortium. https://oncofertility.msu.edu/