Part 2 of a two-part series
Click here to read Part 1: Fertility Preservation Provides Options for Patients With Cancer
How to Talk About Fertility Preservation Options With Young Patients and Their Parents
The American Society of Clinical Oncology’s (ASCO) practice guidelines for fertility preservation in patients with cancer call on health care providers to initiate the discussion on the possibility of infertility with patients with cancer treated during their reproductive years or with parents/guardians of children as early as possible before treatment starts. The guidelines indicate that all oncologic health care providers should be prepared to discuss infertility as a potential risk of therapy.
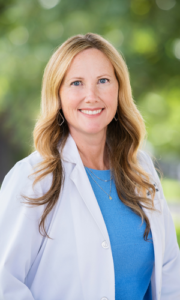
Some programs designate a fertility preservation champion—an advanced practice provider (APP), nurse, or social worker—who may facilitate discussions about fertility and fertility preservation. As the fertility preservation champion at Children’s Hospital Orange County (CHOC), it was the job of Julie A. Messina, PA-C, to talk to the patients and their parents about their options, and to mobilize the members of the team, often within a short period of time, to undertake the necessary steps for fertility preservation to occur. Surgical procedures associated with oocyte harvesting, OTC, TESE, and testicular tissue cryopreservation are typically done at the same time as other procedures, such as placing a port for chemotherapy, a spinal tap, or a tumor biopsy.
“A Plan for Life After Cancer’
When talking with patients and their parents, Messina said she would frame the conversation as wanting to talk to them about preserving their fertility because she wanted to plan for their life after cancer. “By saying that you’re telling them, ‘I believe your child is going to make it’ or ‘I believe you’re going to survive so I want to plan for your life after this.’ When you say it that way it’s able to be processed so they can think about other things than just the shock of their initial diagnosis,” Messina explained.
“I often will start with, ‘There’s a lot of ways to have a family. It doesn’t have to be your eggs, your sperm, your partner’s eggs, your partner’s sperm; there’s donor eggs, there’s adoption.’ From the beginning I want them thinking there’s so many ways to have a family, that in the end if they don’t have their own genetic material, it doesn’t mean they can’t have a family. I tell them, ‘I just want to have all the options available and if we don’t make some choices right now, some of those options may not be available. And you don’t have to use them all but let’s just have them all there.’”
Occasionally a parent and child, usually an adolescent, may disagree about fertility preservation, but the decision is the parent’s legal responsibility, Messina said. Many institutions have a multidisciplinary fertility preservation team, including a psychologist who may counsel the patient and parents, or the case may be referred to the institution’s ethics committee. “In the end we try our very best so that everybody feels good about the decision that they made,” she said.
Messina credited the Oncofertility Consortium with making OTC accessible throughout the United States. If OTC is not available at a particular institution, the Oncofertility Consortium can refer patients to a facility where it is offered and may be able to help with funding as well. The ASCO guidelines for fertility preservation were last updated in 2018. Messina said it will be important for the guidelines to be updated since OTC has become the standard of care.
“Fertility preservation is an important part of survivorship, and I found my job very meaningful to be involved in this small subspecialty,” Messina said. “I would encourage other APPs if they don’t have an oncofertility champion in their facility to get involved with the Oncofertility Consortium and with ECHO to get educated on how to start one. It will be so important to their patients and their patients will be so grateful for them to have done that.”
Resources for APPs
The Oncofertility Consortium hosts an annual conference as well as webinars on topics related to fertility preservation, such as a recent panel discussion on building a comprehensive oncofertility program in pediatrics. ECHO offers a web-based training program that educates allied health providers on the biological, clinical, and psychosocial aspects of fertility preservation for adolescents and young adults. The ECHO course is free for allied health providers, Messina said, and participants who complete the course are equipped to start an oncofertility program and to be the fertility preservation champion at their institution.
Messina moved to Colorado in 2017 and now sees adult patients at Rocky Mountain Cancer Centers. Patients at Mountain Cancer Centers who are interested in fertility preservation program are referred to reproductive endocrinologists. Patients who opt for OTC are referred to the University of Colorado. Messina continues to be involved with the Oncofertility Consortium and ECHO.
For more information
Enriching Communication Skills for Health Professionals in Oncofertility (ECHO). https://echotorch.org/
National Comprehensive Cancer Network. (2023). National Comprehensive Cancer Network Guidelines – Adolescent and Young Adult (AYA) Oncology. https://www.nccn.org/professionals/physician_gls/pdf/aya.pdf
Oktay, K., Harvey, B. E., Partridge, A. H., Quinn, G. P., Reinecke, J., Taylor, H. S., Wallace, W. H., Wang, E. T., & Loren, A. W. (2018). Fertility preservation in patients with cancer: ASCO Clinical Practice Guideline Update. Journal of Clinical Oncology: An American Society of Clinical Oncology Journal, 36(19), 1994–2001.
The Oncofertility Consortium. https://oncofertility.msu.edu/