Glen J Peterson, RN, DNP, ACNP and Jessica Casselberry, MSN, ANP-BC, AOCNP
A thorough assessment of the patient with a hematologic malignancy is essential for the delivery of quality care. Almost every medical condition, symptom or complication will be caused by the patient’s underlying disease, a medication they have been prescribed, or an infection. Taking time to perform an in-depth review of systems (ROS) and physical examination (PE), and focusing on questions specific to the patient’s malignancy, medications, or infectious symptoms is key.
The approach to the ROS and PE should be systematic, from head to toe, completed the same way every time and only modified to expand when needed but never abbreviated. Performing the examination in this manner will aid in the early detection of signs and symptoms that may otherwise lead to complications or even death. Early identification of active or impending complications followed by immediate intervention undoubtedly improves outcomes in patients with blood cancer.
As we complete our ROS and PE, it is also vitally important to review and identify trends in vital signs, body weight, and intake/output. Coupling subjective ROS data and objective PE data with pertinent laboratory and diagnostic testing will complete the puzzle in developing appropriate differential diagnoses for each patient. Considering whether a patient’s complaints or examination findings may be due to their disease, medications, or infections may also help to narrow the list of differential diagnoses.
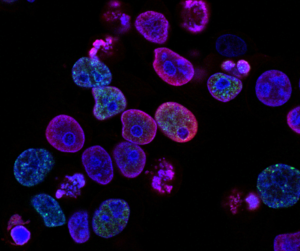
Another variable in the assessment of patients undergoing treatment for a hematologic malignancy is their degree of cytopenias. The depth of neutropenia, lymphopenia, anemia, and thrombocytopenia contributes to the risk of complications and should be considered when evaluating a patient’s clinical scenario. Neutropenia and lymphopenias increase risk of infection in a variety of forms and should guide our attempts to prevent, detect, and treat infection. Anemia increases risk of hypoxia and perfusion-related complications, and efforts to reduce such complications through the use of transfusion support and other interventions are important. Thrombocytopenia increases the risk for bleeding; therefore, protecting patients from trauma and injury, close lab monitoring, and transfusion support are vital.
The management of patients with blood cancer is extremely complex; however, the process by which we gather information about these patients should not be complex. Asking 3 simple questions while performing a systematic and comprehensive examination will help guide and simplify your approach to the management of all patients with hematologic malignancies:
- “Are my patient’s complaints or exam findings due to their disease, a drug they received, or an infection?”
- “Are my patient’s blood counts contributing to their problems?”
- “Are my patient’s symptoms due to having an altered immune system, anemia, or bleeding?”
Whether you have years of experience or are new to the profession, your systematic assessment including PE and ROS will provide a “safety net” in ensuring the highest quality care for your blood cancer patients.

Glen J Peterson, RN, DNP, ACNP

Jessica Casselberry, MSN, ANP-BC, AOCNP.
Division of Hematology, University of Colorado School of Medicine