Karla V. Ow, MSN, FNP, AOCNP
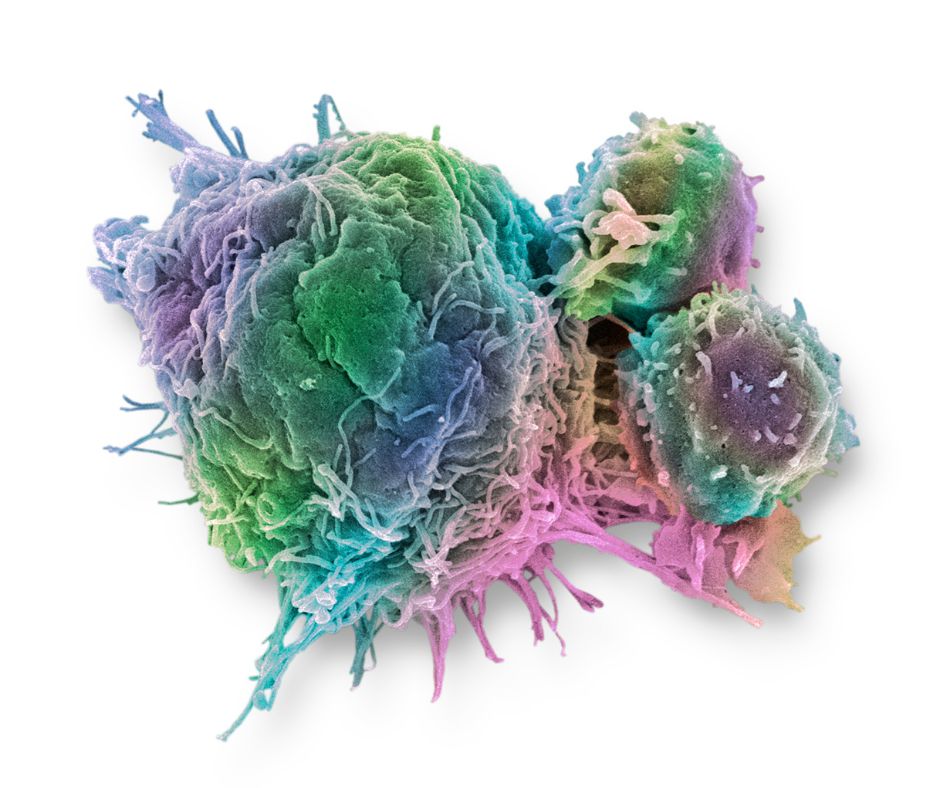
Chimeric antigen receptor (CAR) T cells are lymphocytes that have been genetically modified to produce a CAR that specifically targets tumor cell antigens.1 CAR T-cell therapy has had remarkable response in patients with hematologic malignancies and is currently approved for the treatment of acute lymphoblastic leukemia, lymphomas, and multiple myeloma. Despite unprecedented success, CAR T-cell therapy is associated with serious toxicities that include cytokine release syndrome (CRS) (84% to 93%), immune effector cell-associated neurotoxicity syndrome (ICANS) (18% to 64%), cytopenia (87%), and Grade 3 or 4 infections (18% to 34%).1,2
Risk factors
Risk factors for infection include cytopenia secondary to prior lines of chemotherapy, further lymphodepleting chemotherapy prior to CAR T-cell therapy, the use of steroids for the management of CRS or ICANS, and hypogammaglobulinemia following CAR T-cell infusion.3,4 According to published studies, most infections (40%) occur within the first 90 days after CAR T-cell infusion.4
Bacterial and viral infections are the most common within the first 30 to 60 days of cell infusion.3 Bacterial infections are mostly multidrug resistant bacteria, such as Clostridium difficile and coagulase-negative Staphylococcus, occurring during the neutropenic period, while viral infections include respiratory syncytial virus, influenza, and polyomaviruses.1,4 The incidence of fungal infections is less than 5%, mostly occurring in the period of initial neutropenia or CRS and are mainly candidemia, although several species of molds have been observed to cause lung disease (Aspergillus, Fusarium, Mucorales).1 The most important risk factors for fungal infections are the duration of neutropenia and the prolonged course of systemic corticosteroids prescribed for severe adverse reactions.4 Lastly, many patients have CD4 lymphopenia associated with prolonged B-cell aplasia and reactivation of latent DNA viruses (cytomegalovirus, BK polyomavirus, hepatitis B, and human herpesvirus-6) that are frequently observed 6 to 12 months after CAR T-cell infusion.3
Prophylaxis recommendations
Recommendations for prophylaxis and management strategies for infections after CAR T-cell therapy are largely based on guidelines used for hematopoietic stem cell transplant recipients.1
- For all patients, prophylaxis is recommended for herpes simplex, varicella-zoster, and Pneumocystis jirovecii for up to 1 year after CAR T-cell treatment and/or until a CD4+ >200/μl.1,2
- In addition, antiviral therapy for at least 18 months is recommended for chronic or resolved hepatitis B.1,3,5
- Bacterial and fungal prophylaxis are not prescribed universally after CAR T-cell therapy; however, it should be considered in neutropenic patients along with granulocyte-colony stimulating factor.1,2
- For low-risk patients with no history of invasive fungal infections, treatment with fluconazole is prescribed during the neutropenia period. On the other hand, for high-risk patients with a history of previous fungal infections or high-grade CAR T-cell-associated complications, later-generation antifungal azoles are indicated.1,3
IgG Replacement
Prophylactically replacing immunoglobulin G (IgG) is controversial given the absence of data from randomized clinical trials. At a minimum, screening for serum IgG prior to and the first 3 months post-CAR T-cell therapy for B-cell malignancies should be performed and consider prophylactic intravenous immunoglobulin in patients with continued severe hypogammaglobulinemia (IgG ≤400 mg/dL) and persistent or recurrent respiratory bacterial infections.1,3,5 The role of vaccinations is not yet known, and further studies are needed to guide recommendations.1
CAR T-cell therapy has revolutionized the treatment of hematologic malignancies. A high proportion of patients treated with these targeted therapies experience infectious complications, sometimes secondary to the management of side effects. Screening for latent infections and individualized prophylaxis is advised.

References
- Jain, T., Bar, M., Kansagra, A. J., Chong, E. A., Hashmi, S. K., Neelapu, S. S., . . . Lin, Y. (2019). Use of Chimeric Antigen Receptor T Cell Therapy in Clinical Practice for Relapsed/Refractory Aggressive B Cell Non-Hodgkin Lymphoma: An Expert Panel Opinion from the American Society for Transplantation and Cellular Therapy. Biol Blood Marrow Transplant, 25(12), 2305-2321.
- Chekol Abebe, E., Yibeltal Shiferaw, M., Tadele Admasu, F., & Asmamaw Dejenie, T. (2022). Ciltacabtagene autoleucel: The second anti-BCMA CAR T-cell therapeutic armamentarium of relapsed or refractory multiple myeloma. Front Immunol, 13, 991092.
- Bupha-Intr, O., Haeusler, G., Chee, L., Thursky, K., Slavin, M., & Teh, B. (2021). CAR-T cell therapy and infection: a review. Expert Rev Anti Infect Ther, 19(6), 749-758.
- Wudhikarn, K., Palomba, M. L., Pennisi, M., Garcia-Recio, M., Flynn, J. R., Devlin, S. M., . . . Perales, M. A. (2020). Infection during the first year in patients treated with CD19 CAR T cells for diffuse large B cell lymphoma. Blood Cancer J, 10(8), 79.
- Hill, J. A., & Seo, S. K. (2020). How I prevent infections in patients receiving CD19-targeted chimeric antigen receptor T cells for B-cell malignancies. Blood, 136(8), 925-935.