The Oncology Connection
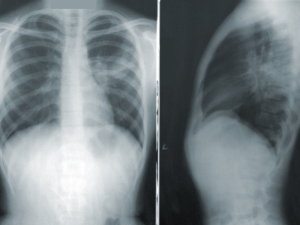
Fam-trastuzumab-deruxtecan-nxki (Enhertu, Daiichi-Sankyo/AstraZeneca), or T-DXd, led to a high intracranial response rate in patients with active brain metastases from human epidermal growth factor receptor 2 (HER2)-positive breast cancer, according to results from the prospective, open-label, single-arm Phase 2 TUXEDO-1 trial.
“The results suggest that T-DXd could be safety used for the treatment of patients with active brain metastases from HER2-positive breast cancer, in case immediate local intervention is not indicated,” the investigators wrote in Nature Medicine. In their discussion of the results, they noted that studies of other breast cancer therapies have yielded disappointing intracranial responses rates.
T-DXd is an antibody-drug conjugate indicated for patients with unresectable or metastatic HER2-positive breast cancer who have received a prior anti-HER2-based regimen.
In the trial, T-DXd was administered intravenously at the standard dose of 5.4 mg/kg bodyweight once every 3 weeks until progression or death or treatment discontinuation. Patients were assessed up to 3 months.
The primary endpoint in the trial was the response rate of brain metastases to T-DXd measured by RANO-BM criteria. Secondary endpoints included progression-free survival (PFS), overall survival (OS), and the safety of T-DXd in patients with active brain metastases.
As of the primary cutoff of December 29, 2021, 15 patients had received a total of 170 cycles of T-DXd. Median follow-up was 12 months (95% confidence interval [CI], 8 months not recorded).
Response to Treatment
In the intent-to-treat population (n=15), intracranial response rate was 73.3% (95% CI 48.1%–89.1%); 2 patients had a complete response (13.3%), 9 patients had a partial response (60%), and 3 had stable disease as the best intracranial response, the investigators reported.
In the per protocol population (n=14), the response rate was 78.6% (95% CI 49.2%–95.3%) (11 out of 14). Two patients had stable disease for 6 or more months, and 1 patient had stable disease at first restaging and progressed after 4 cycles of T-DXd. The clinical benefit rate was 13/14 (92.9%; 95% CI 66.1%–99.8%) in the protocol population.
In patients with extracranial metastases at baseline (n=13), a partial response by RECIST 1.1 was observed in 5 out of 13 patients (27.8%; 95% CI 13.9–68.4%), with the remainder having stable disease. None of the patients progressing on T-DXd had extracranial progression as the first site of progressive disease.
In patients with measurable extracranial disease at baseline (n=8), a partial remission was observed in 5 out of 8 patients (62.5%; 95% CI 24.5–91.5%), with the remainder having stable disease.
PFS and OS
The median PFS was 14 months (95% CI, 11.0 months to not recorded), and the median OS was not reached, according to the investigators. Three patients had died at the 12-month median follow-up: 1 from urosepsis while on treatment and 2 from disease progression. The investigators reported no new safety signals were observed and side effects were consistent with the toxicity profile expected from the pivotal trials.
For more information
Bartsch, R., Berghoff, A.S., Furtner, J., Marhold, M., Bergen, E.S., Roider-Schur, S., Starzer, A.M., Forstner, H., Rottenmanner, B., Dieckmann, K., Bago-Horvath, Z., Haslacher, H., Widhalm, G., Ilhan-Mutlu, A., Minichsdorfer, C., Fuereder, T., Szekeres, T., Oehler, L., Gruenberger, B., Singer, C.F., Weltermann, A., Puhr, R., Presser, M. (2022). Trastuzumab deruxtecan in HER2-positive breast cancer with brain metastases: A single-arm, phase 2 trial. Nature Medicine. https://doi.org/10.1038/s41591-022-01935-8
ClinicalTrials.gov. (2021, February 12 – ). Phase II study of T-DX in HER2-positive breast cancer brain metastases (TUXEDO-1). Identifier NCT04752059. https://clinicaltrials.gov/ct2/show/results/NCT04752059