Beth Sandy, MSN, CRNP, FAPO
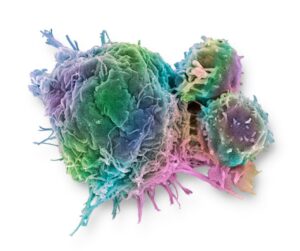
The most common type of squamous cell carcinoma of the head and neck (SCCHN) is oropharyngeal cancer, which arises from the back one-third of the throat, mainly the pharynx. For many years we have known that heavy alcohol use, smoking, and oral tobacco use are significant risk factors for SCCHN. However, over the past decade we have been able to categorize some of these SCCHN cancers by testing the tumor for human papillomavirus (HPV) or more commonly running the immunohistochemistry (IHC) test for p16, the protein commonly increased when HPV is present. The incidence of HPV-positive SCCHN is increasing in younger people in North America; however, it carries a favorable prognosis as compared to HPV-negative SCCHN.1
Most oropharyngeal cancers will be found in the early-stage, locally advanced setting where curative therapy is standard of care. Usual treatment is surgery and, if necessary, adjuvant concurrent chemoradiotherapy. For surgery-ineligible patients, definitive radiation therapy or concurrent chemoradiotherapy is standard of care. Treatment to the oropharynx with radiation and concurrent chemotherapy is very difficult to tolerate, with many toxicities including most frequently: radiation mucositis, radiation dermatitis, myelosuppression, nausea, dysgeusia, and fatigue.
Clinicians began to question this approach: Could we preserve quality of life and minimize toxicity by possibly giving less radiation to patients with HPV-positive oropharyngeal cancer, where the prognosis and cure rates were historically superior to patients without HPV-positive disease? This led to clinical trials looking at administering a de-escalated course of radiation in nonrandomized studies. Two studies were recently presented at the 2024 Multidisciplinary Head and Neck Cancers Symposium.
One study performed at Washington University School of Medicine looked at postoperative de-escalated radiation using either radiation alone or radiation with chemotherapy in patients who had an HPV-associated oropharyngeal cancer and were not considered high risk. In this study, patients had significantly less weight loss (4.9%) than usually seen in conventional radiation doses of a similar historical cohort (7.9%) and a 4-year progression-free survival (PFS) of 90%, similar to conventional PFS rates in this setting.2
Another nonrandomized study of HPV-associated oropharyngeal cancer in the locally advanced, inoperable setting, from the University of Michigan, used de-intensified radiation from 70 Gy to 54 Gy in patients who were showing good responses (at least a 50% reduction in metabolic tumor volume) midway through their chemoradiotherapy course by using positron emission tomography (PET) scan imaging. Other patients who did not experience this tumor reduction remained on radiation to complete the 70 Gy course. The 2-year PFS in these groups were 87% for the group of patients who received 70 Gy vs. 84% for the group of patients who received only the 54 Gy. Also seen in this trial was a reduction in weight loss, with patients in the 54 Gy cohort experiencing an average of 6% weight loss as opposed to 12.6% for the 70 Gy cohort, with 5% fewer patients needing a nasogastric tube in the 54 Gy cohort.3
Treatment for SCCHN has many challenges and patients experience terrible, often disfiguring side effects. Based on these early study results, future clinical trials should be developed in a randomized fashion to evaluate if these HPV-associated oropharyngeal cancers could be spared excess radiation. Perhaps these patients could experience less side effects even beyond weight loss, including mucositis and dermatitis. This remains to be seen, but these 2 trials certainly give hope that maybe in the future, this could offer patients a less toxic treatment course.

Beth Sandy, MSN, CRNP, FAPO, is a thoracic oncology nurse practitioner at Abramson Cancer Center, University of Pennsylvania, Philadelphia. She is the editor-in-chief of The Oncology Connection.
References
- Chow L. Q. M. (2020). Head and Neck Cancer. The New England journal of medicine, 382(1), 60–72. https://doi.org/10.1056/NEJMra1715715
- Thorstad W. L., Jackson, R. S., Oppelt, P., et al. (2024). Long-term efficacy of risk-directed de-escalated post-operative adjuvant therapy for surgically resected locally advanced, human papillomavirus-positive oropharynx squamous-cell carcinoma: A non-randomized, multi-arm phase 2 trial. 2024 Multidisciplinary Head and Neck Cancers Symposium. Abstract 14. Presented March 1, 2024.
- Regan, S. N., Rosen, B. S., Suresh, K., et al. (2024). FDG-PET-based selective de-escalation of radiotherapy for HPV-related oropharynx cancer: Results from a phase II trial. 2024 Multidisciplinary Head and Neck Cancers Symposium. Abstract 16. Presented March 1, 2024.